Tips for Best Practices on Absent Transformation Zone
Post date: November 15, 2024
Reviewed by: Daniel Chernaev, MD
Cervical intraepithelial neoplasia (CIN)/intraepithelial lesions (LSIL/HSIL) are likely to occur in the cervical transformation zone. The transformation zone is located outside of the squamocolumnar junction (SCJ), between the original SCJ (usually not visible on colposcopy) and the current SCJ (Figure 1).
The cytology report comments on both the presence of cells from the transformation zone or endocervix and the cytologic appearance of the squamous epithelial cells. Factors that may impact the presence of endocervical/transformation zone cells on a specimen include bacterial or candidal infections, patient age, parity, and pregnancy.
In the past, the absence of endocervical cells/transformation zone was thought to reflect the adequacy of the specimen; however, subsequent studies have found that the lack of endocervical cells/transformation zone does not increase the risk of subsequent histologic high-grade lesion, and some studies have found a lower risk of CIN3+ in patients without a transformation zone compared to those with a transformation zone present.
From a clinical utility standpoint, the absence of the transformation zone does little to change how clinicians manage results. Management of negative for intraepithelial lesion or malignancy (NILM) cytology results with absent endocervical cells/transformation zone depends on the age of the patient and whether or not a concurrent HPV test was done (Figure 2).
If the patient is 21-29 years old, routine age-based screenings should continue.
If the patient is ≥ 30 years old, management depends on HPV result.
- If HPV testing was not performed, the preferred next step is HPV testing of the specimen. If that is not possible, then cytology is repeated in 3 years.
- If the HPV testing is negative, routine age-based screening should be continued.
- If the HPV testing is positive, the recommendation is to either repeat HPV-based testing in 1 year or perform HPV genotyping and triage further based on the results.
Overall, these recommendations are unchanged from the 2012 management guidelines.
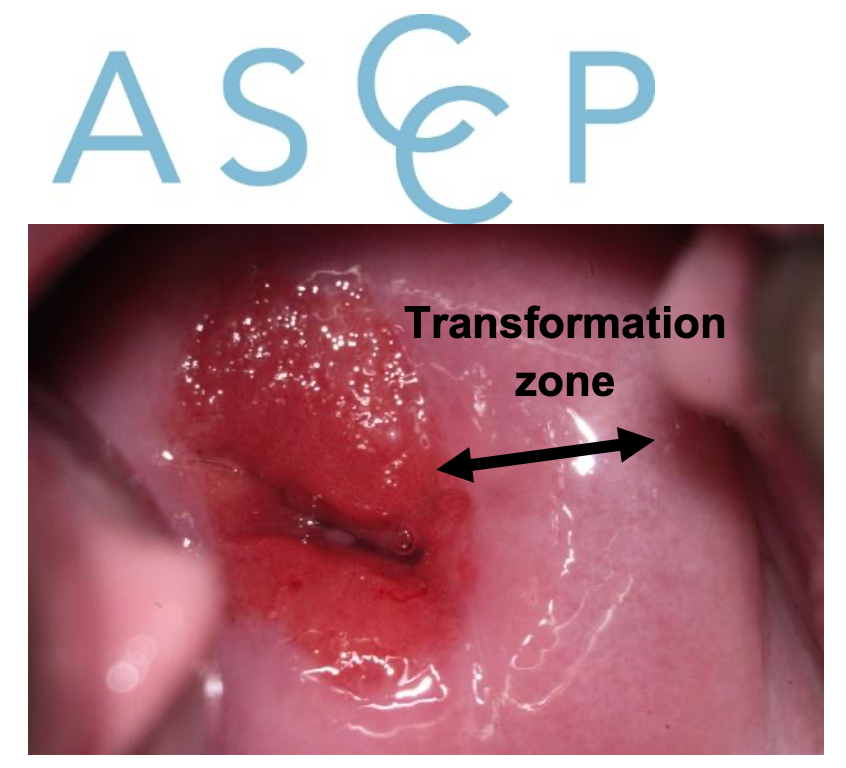
Figure 1. Cervix showing the location of the transformation zone (double-headed arrow).

Figure 2. Management of negative for intraepithelial neoplasia or malignancy (NILM) cytology with absent transformation zone or endocervical cells (adapted from Figure 6 of Perkins et al, 2019 ASCCP Risk-Based Management Consensus Guidelines for Abnormal Cervical Cancer Screening Tests and Cancer Precursors).
As primary HPV testing becomes more widely available, this topic will likely become increasingly less relevant.
Download PDF